Tb Test Form Templates
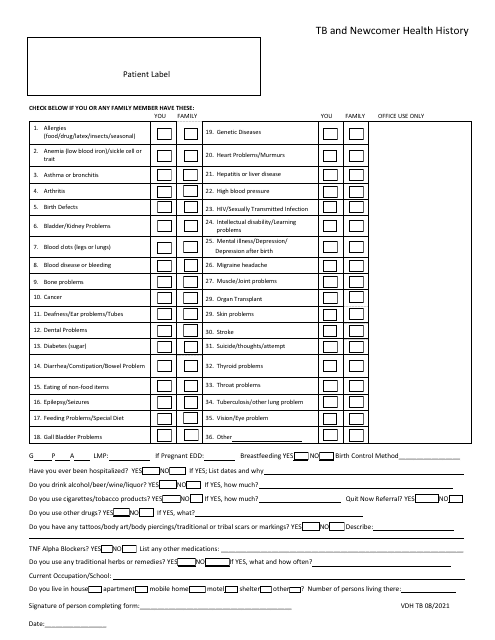
Tb Test Forms are used to record the results of a tuberculosis (TB) test. They are typically used by healthcare professionals to document the presence or absence of a TB infection in an individual. The form includes information such as the test date, the method used, and the results of the test.
Documents:
12
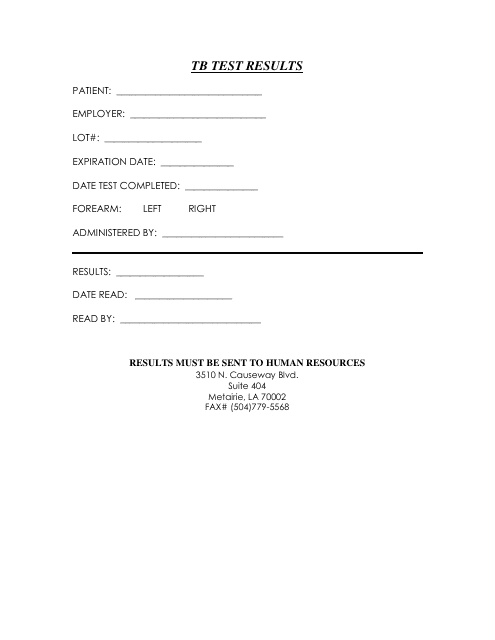
This form is used for documenting the results of a TB (tuberculosis) test. It provides a record of whether the person being tested has been found to be positive or negative for TB infection.
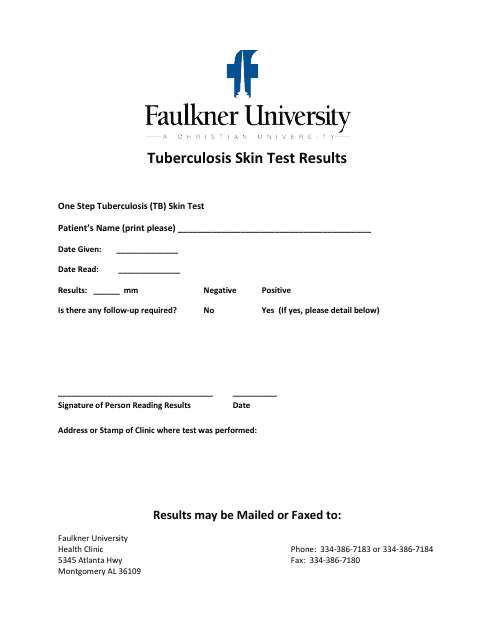
This document provides information about the Tuberculosis Skin Test results at Faulkner University in Alabama.
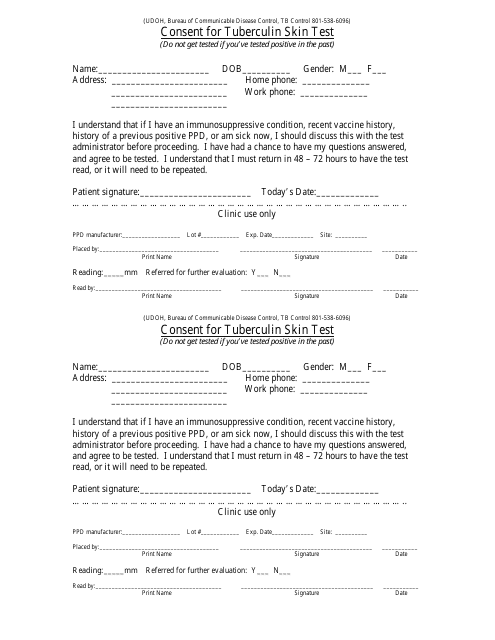
This Form is used for obtaining consent from individuals in Utah for a Tuberculin Skin Test, a common diagnostic test for tuberculosis.
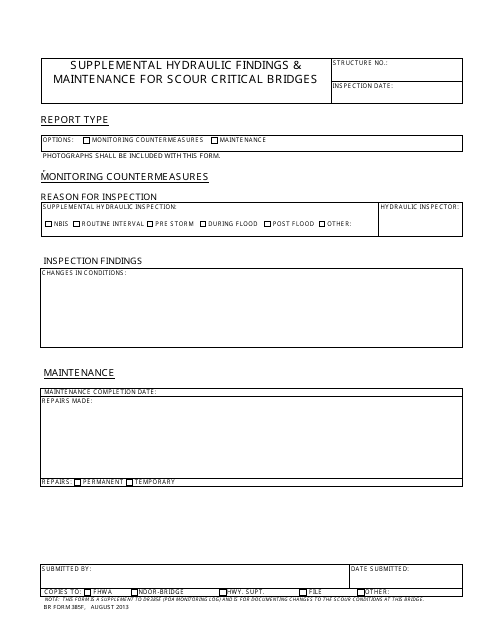
This form is used for documenting supplemental hydraulic findings and maintenance activities related to scour critical bridges in Nebraska.
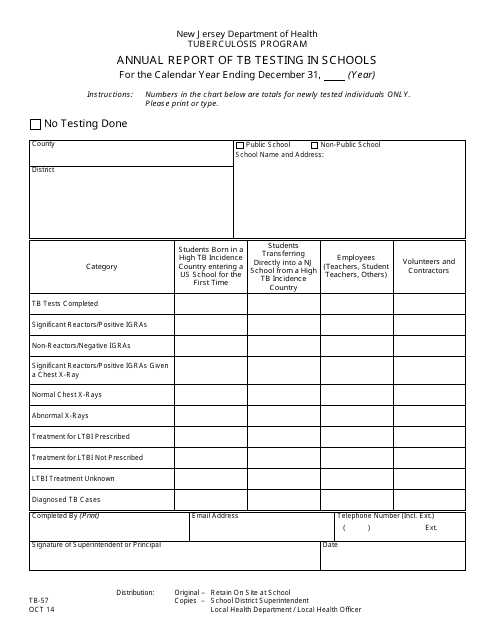
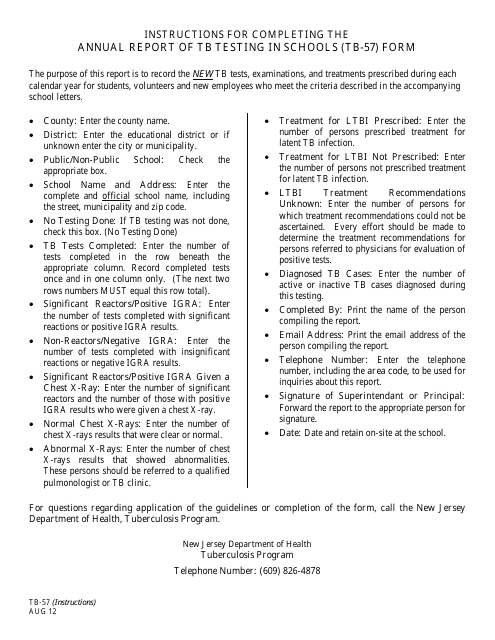
This document is used for reporting annual tuberculosis testing in schools in the state of New Jersey.
This Form is used for submitting the annual report of TB testing in schools in New Jersey. It provides instructions on how to complete and submit the report.
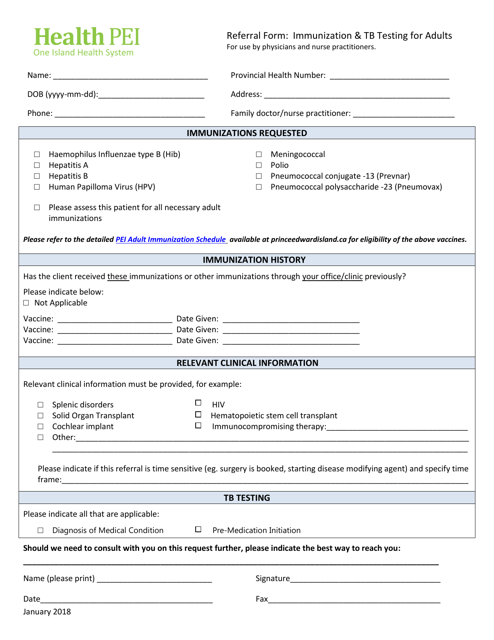
This form is used to refer adults in Prince Edward Island, Canada for immunization and TB testing.
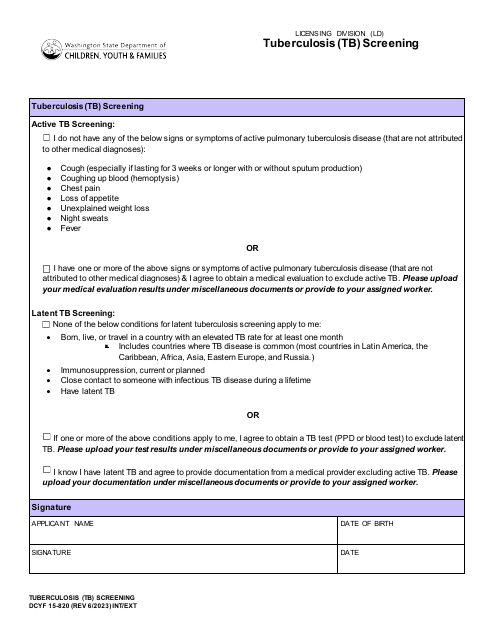
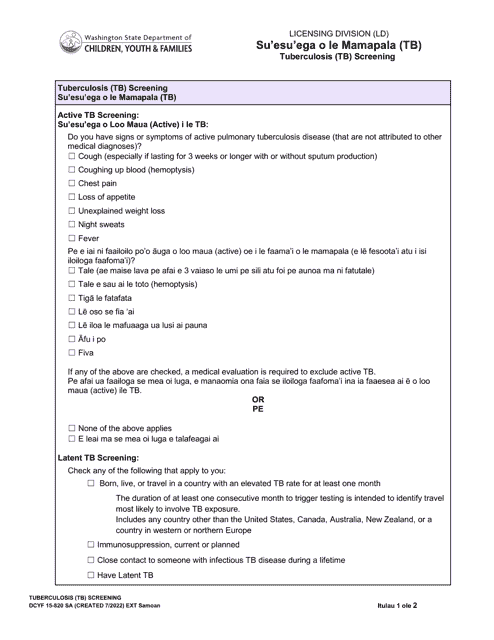
This form is used for Tuberculosis (TB) screening in Washington state for English and Samoan speakers.
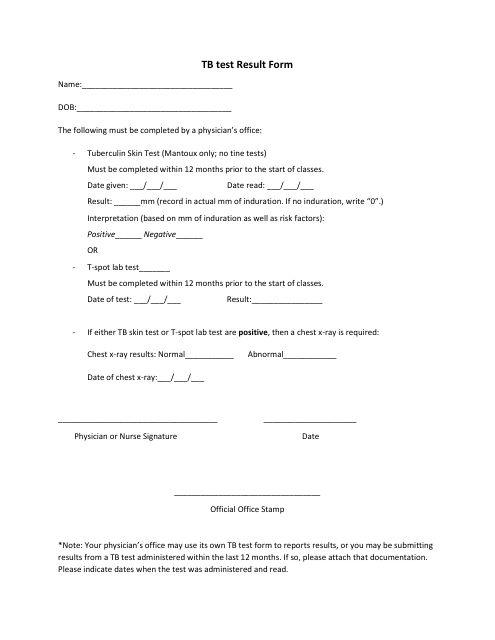
This document is used for recording the results of a Tuberculosis (TB) skin test, often conducted by healthcare providers, to assist in determining whether an individual has been infected with the TB bacteria.
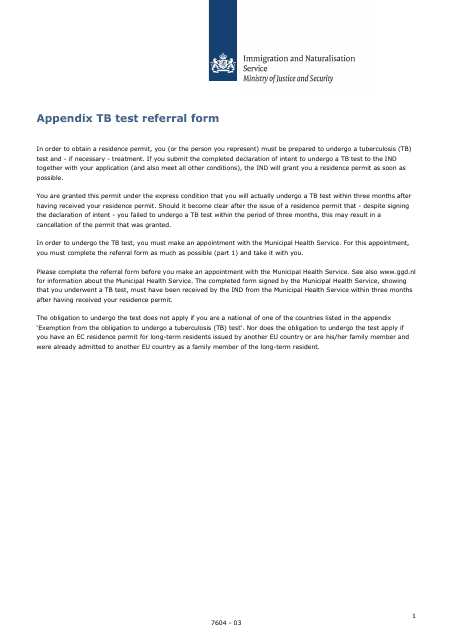
This form is used to refer individuals in the Netherlands for tuberculosis testing. It fosters streamlined communication between healthcare professionals to ensure timely and appropriate testing for potential TB patients.