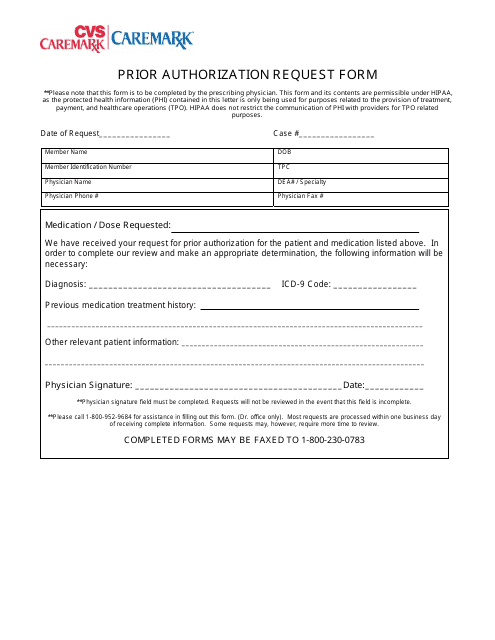
Caremark Prior Authorization Form Templates
The Caremark Prior Authorization Form is used to request approval from Caremark, a pharmacy benefit manager, for coverage of certain medications or services that may require prior authorization. This form is typically used when a medication or treatment is not automatically covered by the patient's insurance plan and requires additional documentation or review before they will provide coverage.
Documents:
1
This Form is used for requesting prior authorization for medications through CVS Caremark.