Express Scripts Prior Authorization Form Templates
Express Scripts Prior Authorization Form is used for requesting approval from Express Scripts, a pharmacy benefit manager, for the coverage of certain medications or medical treatments. Prior authorization is required when a medication or treatment is not automatically covered by an individual's insurance plan and needs further review to determine if it meets the necessary criteria for coverage. The purpose of the form is to gather information about the patient, prescriber, medication, and medical condition so that Express Scripts can make an informed decision regarding coverage.
Documents:
7
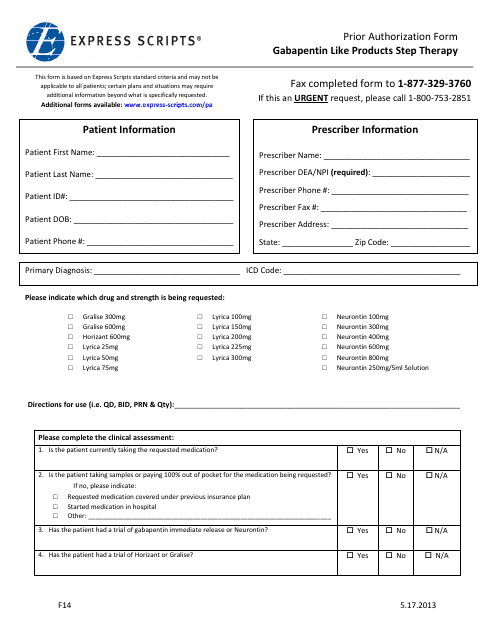
This form is used for requesting prior authorization for Gabapentin-like products through Express Scripts' step therapy program.
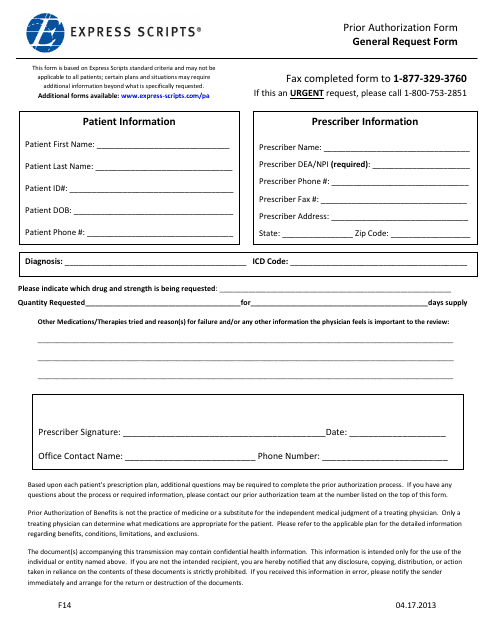
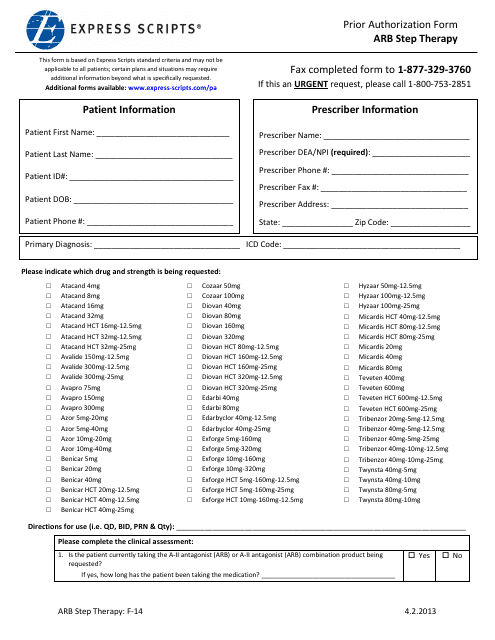
This form is used for requesting prior authorization from Express Scripts for medications or medical treatments.
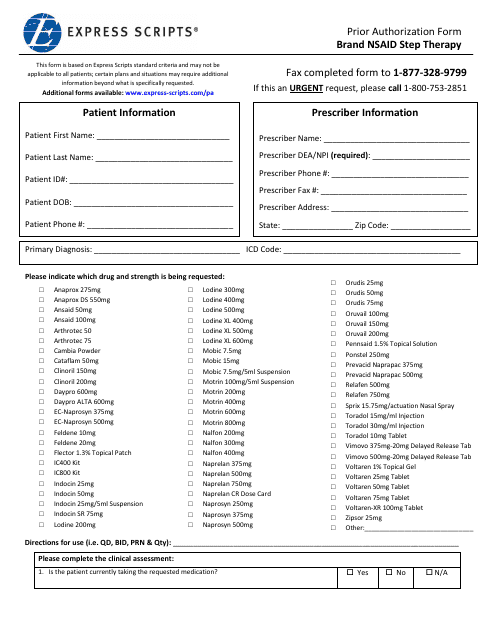
This Form is used for requesting prior authorization for brand name nonsteroidal anti-inflammatory drugs (NSAIDs) as part of step therapy process through Express Scripts.
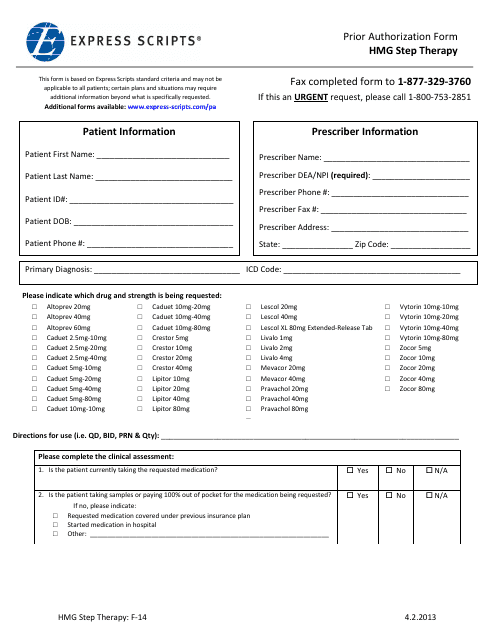
This form is used for requesting prior authorization for HMG step therapy through Express Scripts.
This form is used for obtaining prior authorization for step therapy through Express Scripts. Step therapy is a cost-saving measure that requires patients to try lower-cost medications before progressing to more expensive options.
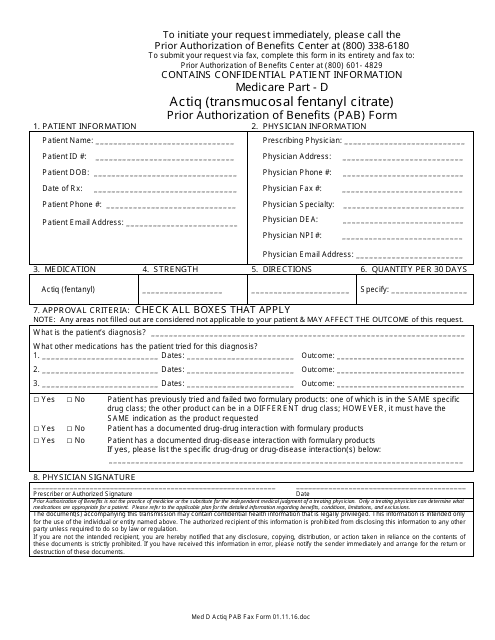
This Form is used for requesting prior authorization of benefits for Actiq (Transmucosal Fentanyl Citrate) under Medicare Part D through Express Scripts.
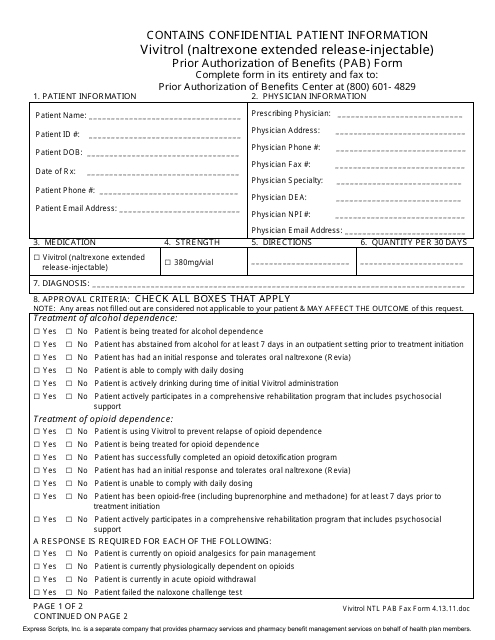
This Form is used for requesting prior authorization of benefits for Vivitrol, a medication for alcohol and opioid dependence. It is an extended-release injectable form of naltrexone.