United Healthcare Prior Authorization Form Templates
United Healthcare Prior Authorization Forms are used to request approval from United Healthcare for certain health care services or medications that may require pre-authorization. This form helps ensure that the requested services or medications are medically necessary and meet the coverage criteria established by United Healthcare. The purpose of prior authorization is to determine if the requested services or medications are eligible for coverage before being provided, which helps manage costs and ensure appropriate utilization of healthcare resources.
Documents:
3
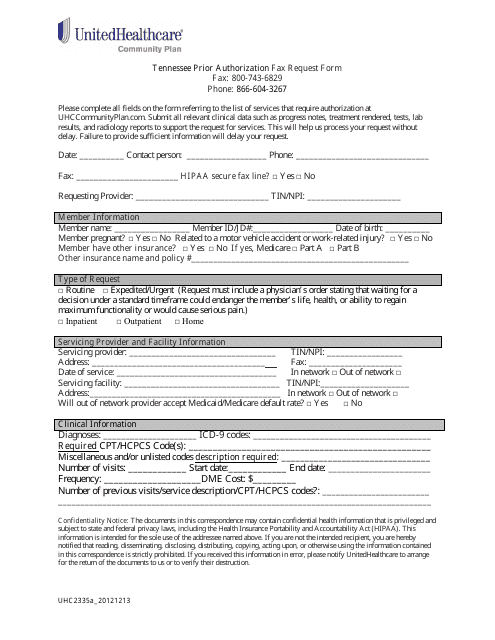
This form is used for requesting prior authorization for healthcare services with UnitedHealthcare in the state of Tennessee.
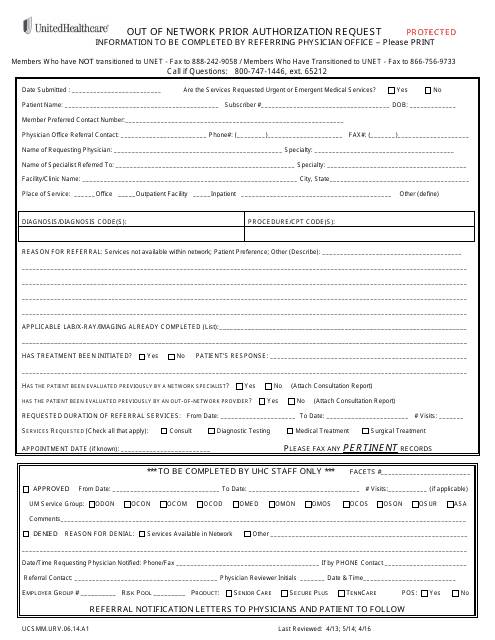
This document is a form used by Unitedhealthcare to request prior authorization for out-of-network healthcare services.
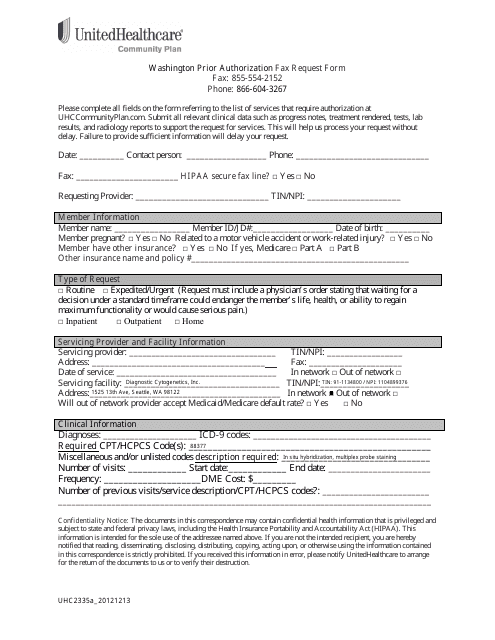
This Form is used for requesting prior authorization for healthcare services from UnitedHealthcare in Washington.