Priority Health Prior Authorization Form Templates
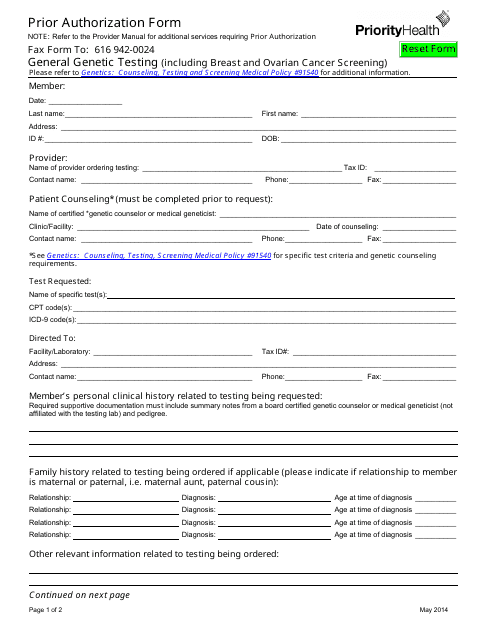
The Priority Health Prior Authorization Form is used to request authorization from Priority Health for certain medical services, procedures, or medications. It is typically required when a healthcare provider wants to confirm coverage and obtain approval before proceeding with the requested treatment or prescription. This form helps ensure that the services or medications are deemed medically necessary and covered by Priority Health insurance.
Documents:
1
This form is used for requesting prior authorization from Priority Health for certain medical treatments or services.