Medicaid Prior Authorization Form Templates
Medicaid Prior Authorization Forms are used to request approval from Medicaid for certain medical services, procedures, medications, or equipment that require prior authorization before they can be covered by the Medicaid program. This process ensures that the requested services or items meet the necessary criteria and are deemed medically necessary for the specific patient. By completing the form, healthcare providers can seek approval for their patients' healthcare needs and determine if Medicaid will cover the cost.
Documents:
1
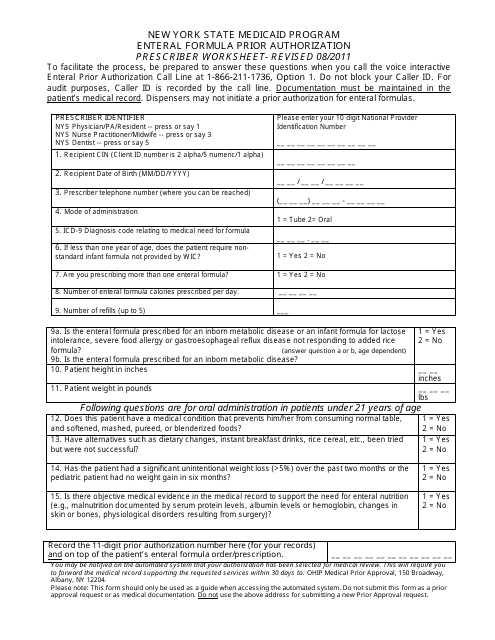
This Form is used for prior authorization of enteral formula prescription in the New York State Medicaid Program.