Medicare Prior Authorization Form Templates
Medicare Prior Authorization Forms are used to request approval from Medicare for certain medications, procedures, or services. They ensure that the requested medical intervention is necessary and appropriate before Medicare provides coverage. These forms help control costs and ensure that Medicare resources are used efficiently and effectively.
Documents:
2
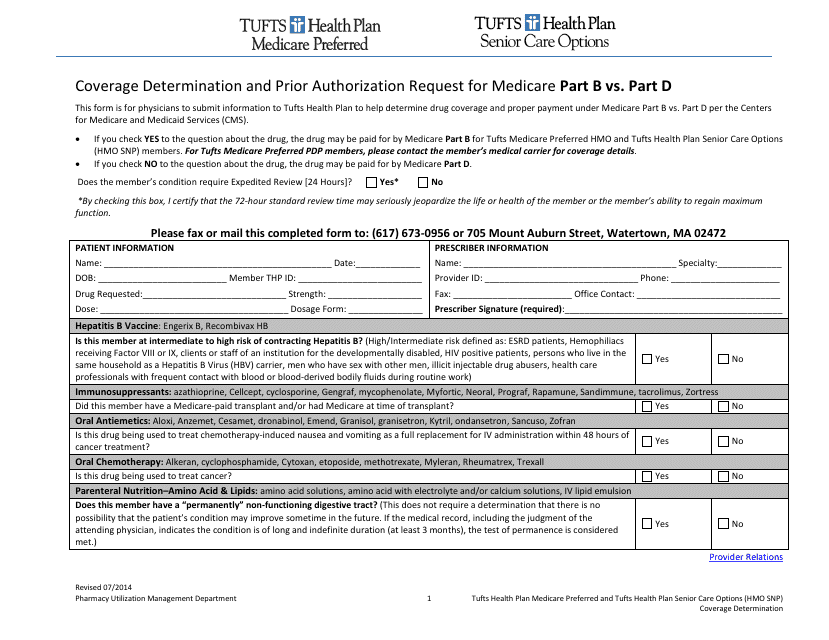
This Form is used for submitting a coverage determination request or prior authorization request for Medicare Part B or Part D benefits under Tufts insurance.
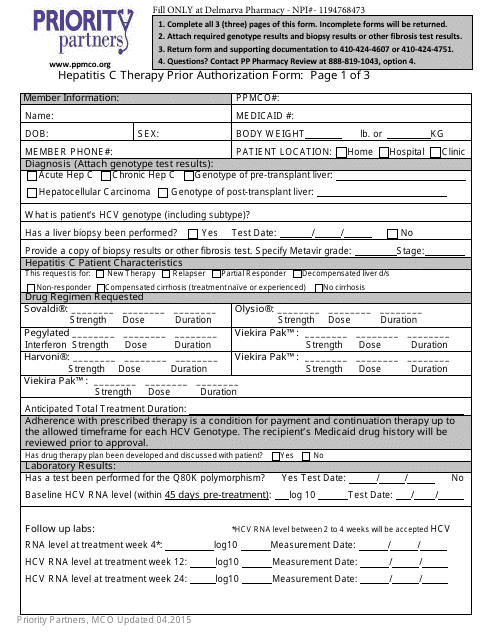
This form is used to request prior authorization for Hepatitis C therapy with Priority Partners.