Prescription Coverage Templates
Prescription Coverage: Ensuring Access to Medications
In today's healthcare landscape, having adequate prescription coverage is essential. It provides individuals with access to the medications they need to manage their medical conditions and improve their overall well-being. Prescription coverage offers financial protection by helping to offset the cost of medications, making them more affordable and accessible to those who need them.
At the heart of prescription coverage are various documents and resources that help individuals navigate through the healthcare system and obtain the medications they require. These documents, also known as prescription coverage forms, play a crucial role in ensuring that individuals receive the appropriate medications and eliminate any barriers that may exist.
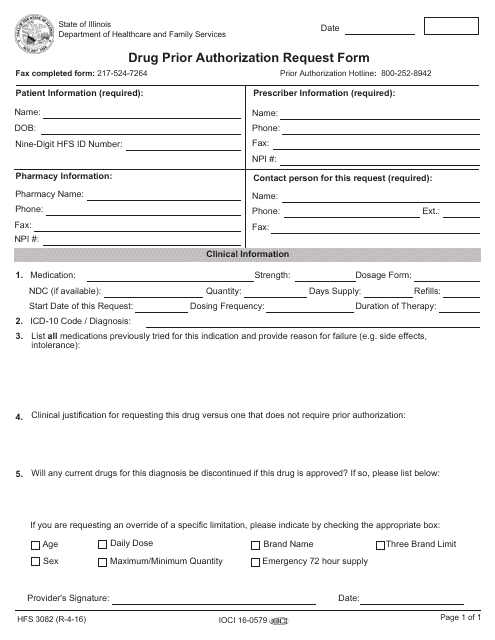
Whether it's the Form HFS3082 Drug Prior Authorization Request Form in Illinois or the Instructions for Rhode Island Medicaid Prior Authorization Form, these documents streamline the process of obtaining prescription medications. They provide a clear and concise outline of the necessary steps to take, making it easier for individuals to navigate through the complexities of prescription coverage.
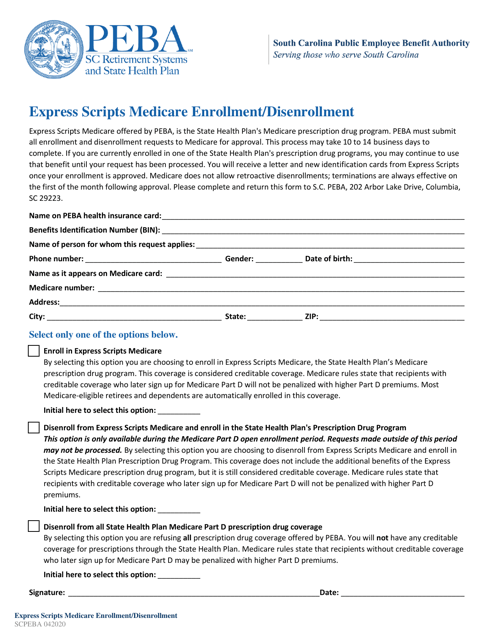
Additionally, documents like the Express Scripts Medicare Enrollment/Disenrollment form in South Carolina or the Prescription Drug Claim Form in Washington simplify the administrative tasks associated with prescription coverage. These documents serve as a means to enroll or disenroll from prescription coverage programs, ensuring that individuals have access to the medications they need without any unnecessary delays or complications.
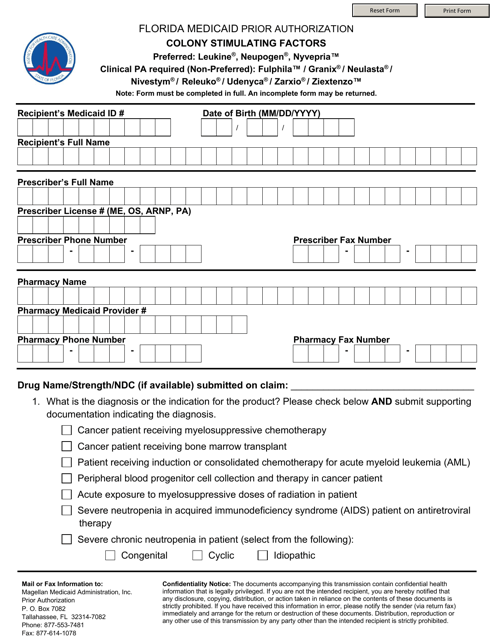
Medicaid beneficiaries also benefit from documents like the Florida Medicaid Prior Authorization for Colony Stimulating Factors. This document addresses specific medication needs and ensures that individuals receive the necessary approvals for medications that may have special criteria for coverage.
Prescription coverage documents provide a comprehensive and efficient way to manage medication needs, taking into account the unique requirements of each individual. They serve as invaluable resources, helping individuals navigate the complex world of prescription coverage and ensuring access to necessary medications.
If you're in need of prescription coverage or have questions about the eligibility criteria for certain medications, these documents are indispensable tools. Browse our collection of prescription coverage forms to find the specific documents that align with your needs, and take the first step towards accessing the medications you require.
Documents:
19
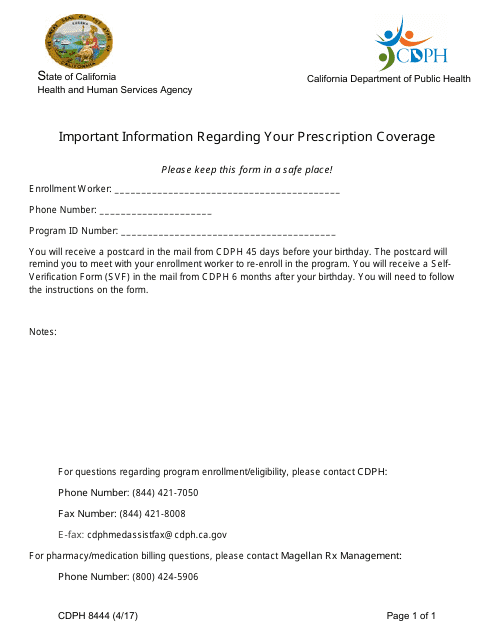
This form provides important information about your prescription coverage in the state of California. It includes details about your insurance plan, pharmacy benefits, and how to access prescription medications.
This Form is used for submitting prescription drug information in the state of Nevada.
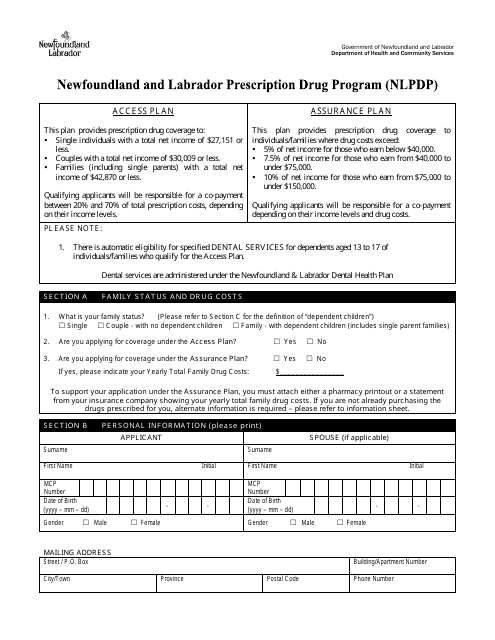
This document is an application form for the Newfoundland and Labrador Prescription Drug Program (NLPDP) in Canada. It is used to apply for coverage for prescription drugs in the province of Newfoundland and Labrador.
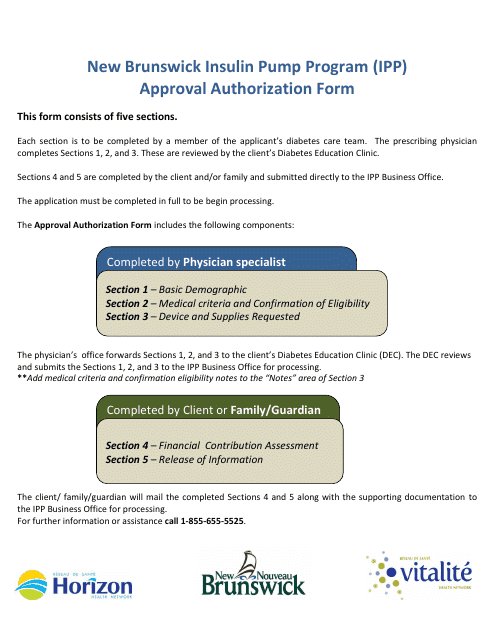
This Form is used for obtaining approval for the Insulin Pump Program (IPP) in New Brunswick, Canada.
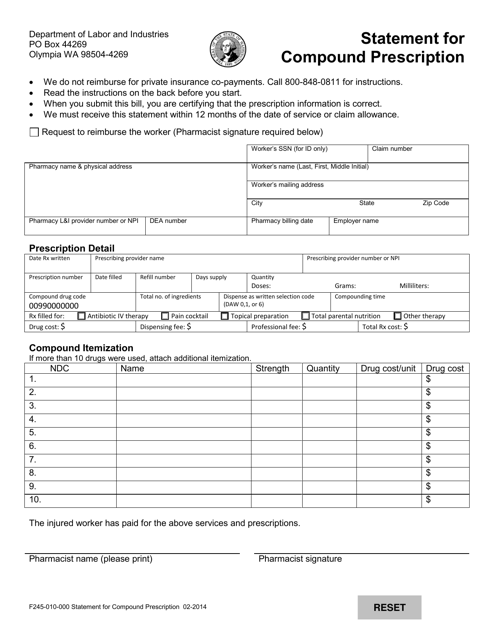
This form is used for providing a statement for compound prescription in the state of Washington. It is required for compounds that are custom-made medications.
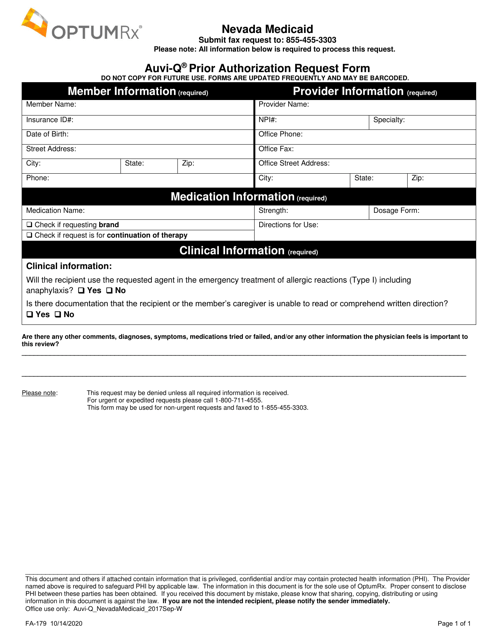
This Form is used for requesting prior authorization for Auvi-Q medication in the state of Nevada.
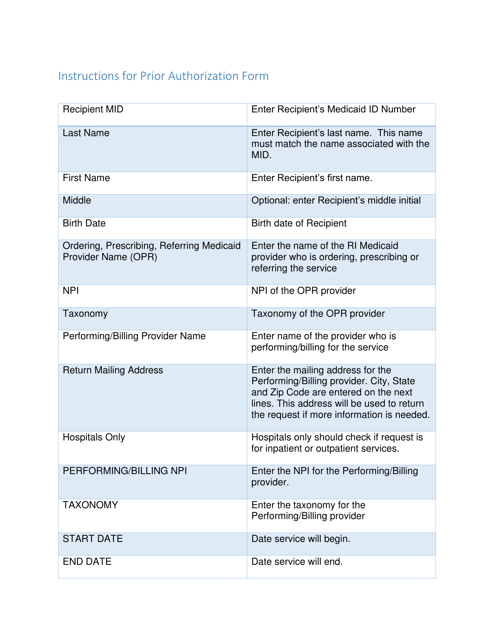
This document provides instructions for completing the Rhode Island Medicaid Prior Authorization Form. It is used to request approval for specific medical services or treatments before they can be covered by Medicaid in Rhode Island.
This Form is used for enrolling or disenrolling in the Express Scripts Medicare plan in South Carolina.
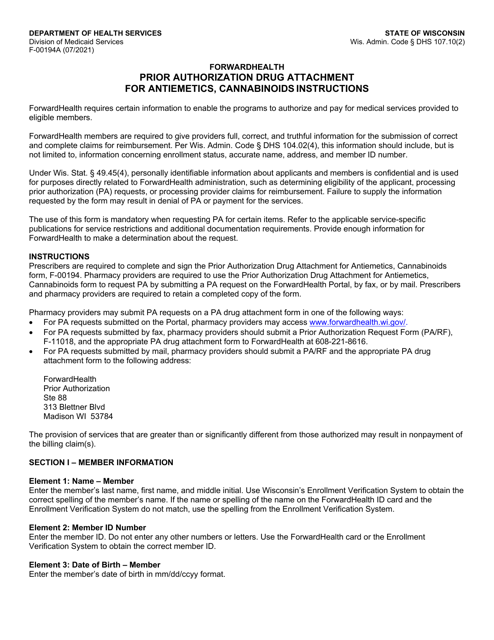
This Form is used for submitting a prior authorization drug attachment for antiemetics and cannabinoids in the state of Wisconsin. It provides instructions on how to complete and submit the form for approval.
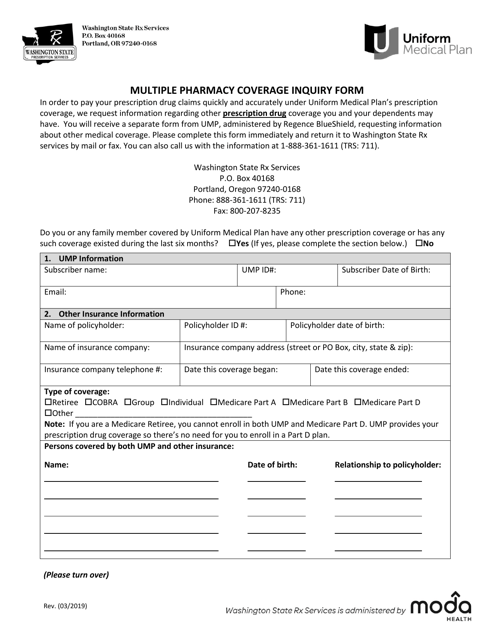
This form is used for inquiring about multiple pharmacy coverage in the state of Washington.
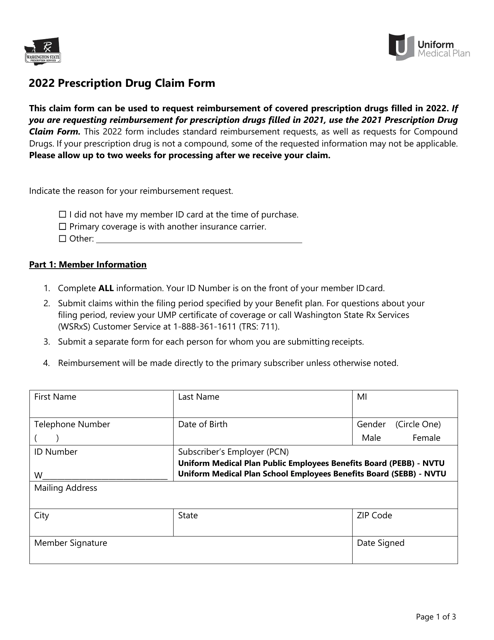
This form is used for filing prescription drug claims in the state of Washington. It allows individuals to seek reimbursement for the cost of prescribed medications.
This form is used for Medicaid patients in Florida who need prior authorization for colony stimulating factors.
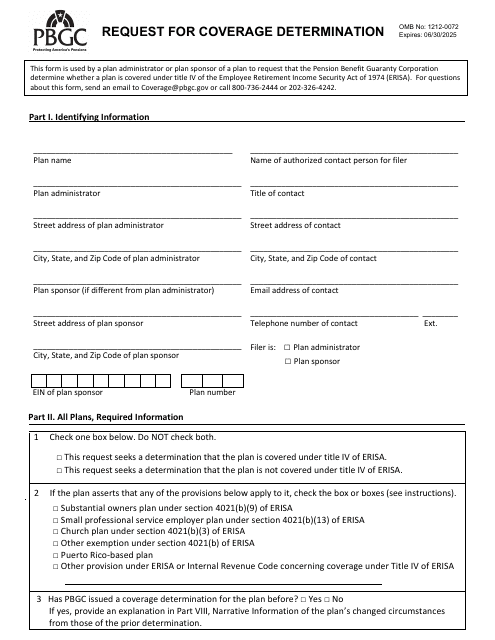
This document is used to request a determination of coverage for an insurance claim or benefit. It typically involves submitting information and evidence to support the request and may be required by the insurance company before they make a decision on coverage.
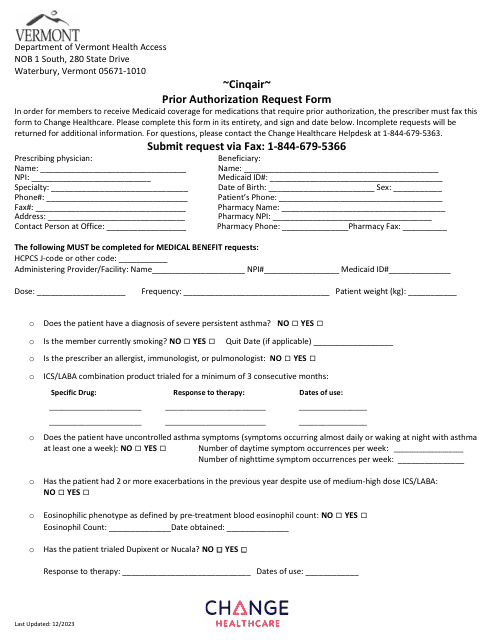
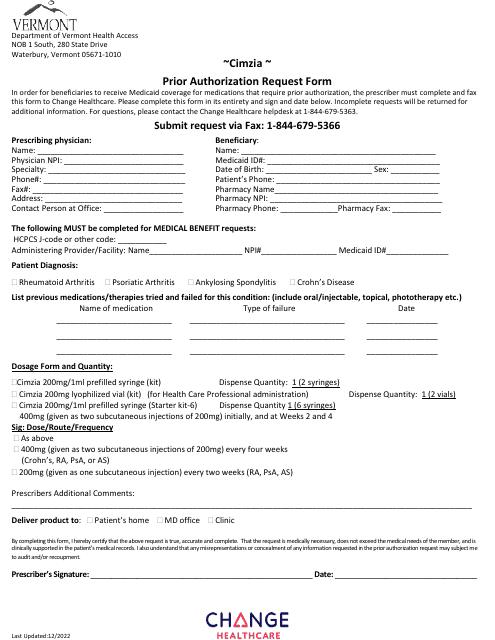
This Form is used for submitting a prior authorization request for Cimzia medication in the state of Vermont.
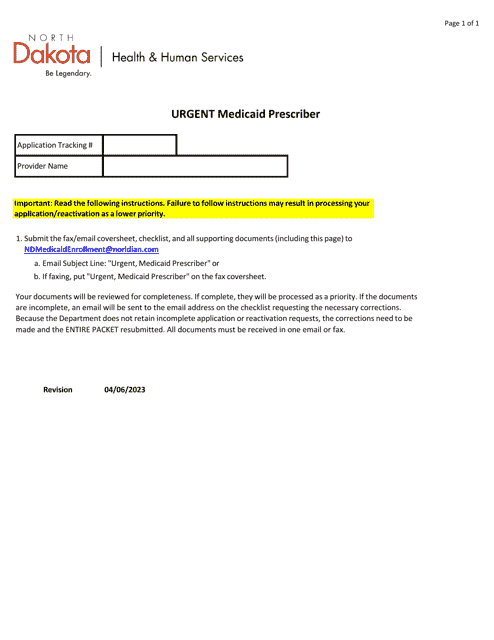
This document is for healthcare providers in North Dakota who need to urgently apply to be a Medicaid prescriber.
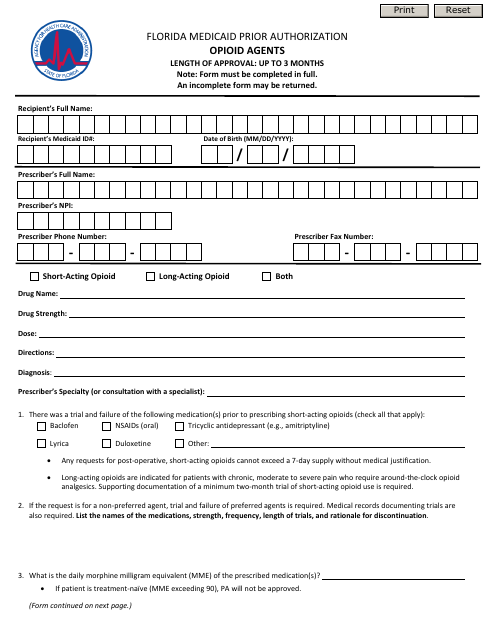
This form is used for obtaining prior authorization for opioid agents under Florida Medicaid in the state of Florida.